
Respondents
The survey was completed by 39 respondents from 14 regions (see Appendix): Abruzzo (n = 2), Campania (n = 2), Emilia-Romagna (n = 4), Friuli Venezia Giulia (n = 2), Lazio (n = 3), Liguria (n = 1), Lombardy (n = 10), Marche (n = 1), PA Bolzano (n = 1), Piedmont (n = 1), Sardinia (n = 1), Sicily (n = 2), Tuscany (n = 1), and Veneto (n = 9). The overall response rate was 23%, with significant variation across regions: while some areas, such as Veneto and the Autonomous Province of Bolzano, achieved full participation (100%), regions like Puglia, Calabria, and Basilicata did not register any responses (0%). Despite this seemingly modest percentage, it is consistent with response rates typically observed in similar survey-based studies [23, 24].
The sample, as illustrated in Table 1, includes healthcare organizations from all major geographic areas of Italy—Northwest, Northeast, Central Italy, South, and Islands—ensuring that the findings capture the diversity of healthcare settings across the country. This includes regions with varying levels of infrastructure, resources, and organizational autonomy. The notable overrepresentation of Northern regions (Northwest and Northeast, accounting for 72% of the sample) reflects the actual concentration of healthcare infrastructure and resources in these areas. This aligns with well-documented geographic disparities within the Italian healthcare system, where Northern regions typically exhibit more advanced and systematically implemented sustainability practices. In terms of organizational diversity, the sample is well-structured, with Local Health Authorities comprising 62% of respondents, consistent with their central role in delivering healthcare at the regional level. The inclusion of Hospital Trusts and IRCCS (38% collectively) further enriches the analysis by incorporating the perspectives of research-focused and tertiary care institutions, ensuring a broader representation of organizational priorities and capacities.
The respondents primarily hold management roles or are professionals specifically appointed by organizational leadership due to their responsibilities or particular interest in environmental sustainability. A significant share (16 respondents) is involved in strategic governance, including positions such as general, medical, or administrative directors. Furthermore, a considerable number of participants occupy technical and operational positions, particularly within units dedicated to infrastructure management, clinical engineering (10 respondents), and organizational or technological innovation (6 respondents). The remaining respondents are engaged in specialized departments focusing on areas such as prevention and environmental safety.
The progression of healthcare organizations in embedding environmental sustainability.
Table 2 maps the progression of healthcare organizations in embedding environmental sustainability (ES), following the adapted stages of Rogers’ innovation-decision model. 97% (38 out 39) of respondents reported that top management had acknowledged the relevance of ES in organizational management, suggesting high levels of awareness and positive attitudes toward sustainability within leadership teams. However, only sixteen (41%) organizations had formalized their commitment to ES in strategic documents, reflecting a gap between awareness and formal strategic integration. Despite this, thirty-five (90%) respondents indicated that their organizations had already taken concrete actions related to ES, demonstrating that most organizations are actively engaged in sustainability practices even without formalized strategic commitments.
The establishment and dissemination of environmental sustainability objectives
Of the 16 participants who reported having formally expressed their intention to work on environmental sustainability, only 12 submitted the required documentation. The analysis of the 12 strategic documents provided by healthcare organizations highlights a clear distinction between general governance documents and dedicated sustainability-focused documents, as detailed in Table 3.
The majority (9 documents) included references to ES within institutional frameworks such as the Integrated Plan of Activities and Organization (PIAO) or the Corporate Act. Both are mandatory governance tools for Italian public healthcare entities, designed to define organizational structure, strategic objectives, and compliance with transparency and performance regulations. In these cases, sustainability is typically addressed as part of broader institutional principles, resulting in high-level commitments without detailed operational strategies. By contrast, a smaller number of organizations produced dedicated sustainability documents, including two Sustainability Reports and one project-specific document explicitly focused on environmental objectives. These documents generally present more concrete initiatives, measurable actions, and long-term planning, reflecting a more proactive approach to sustainability beyond formal compliance. Across all documents, recurring themes emerged, particularly in areas such as energy efficiency, waste management, digitalization, structural modernization, sustainable mobility, and green procurement. These priorities indicate a shared awareness of key environmental challenges within the healthcare sector. However, despite these common thematic areas, the depth and operationalization of sustainability strategies varied considerably. While a few organizations demonstrated structured approaches supported by performance indicators, many limited their engagement to general statements without clear implementation plans. This analysis suggests that, although environmental sustainability is increasingly acknowledged at a strategic level, only a limited number of healthcare organizations have developed specialized documentation that enables a deeper and more operational integration of sustainability practices.
Governance and competence in environmental sustainability
The data reveal that 28 of the 35 organizations actively pursuing environmental sustainability efforts have implemented organizational measures. Among these, 12 organizations have recruited specialized technical personnel, emphasizing the growing recognition of the importance of expertise in addressing sustainability challenges. Additionally, 6 organizations have established multidisciplinary teams, reflecting a collaborative approach necessary for tackling the multifaceted nature of sustainability. In other cases, organizations have pragmatically assigned sustainability responsibilities to existing staff, relying on internal resources to meet environmental goals. While this approach demonstrates adaptability, it also underscores potential resource constraints, which could limit the long-term effectiveness of sustainability initiatives. The professional backgrounds of individuals involved in sustainability efforts reveal a pronounced emphasis on technical expertise. Engineering professionals, numbering 33, represent the majority, signaling a focus on technical and infrastructural solutions such as energy efficiency, waste management, and system optimization. Beyond engineering, representation from Medicine (11 professionals), Economics and Management (11 professionals), and Pharmacy (4 professionals) highlights efforts to embed sustainability into clinical operations and organizational management. Additional contributions from fields such as Law (3 professionals), Chemistry (1 professional), and Prevention Technicians enrich the governance framework, supporting compliance, chemical waste management, and risk mitigation.
The implementation of ES in healthcare organizations
The questionnaire examined how each participating healthcare organization implemented ES across the core areas defined by the Green Plan model. Figure 1 illustrates the prioritization of environmental sustainability initiatives by healthcare organizations in Italy, highlighting the number of organizations working on each area out of a total of 35.
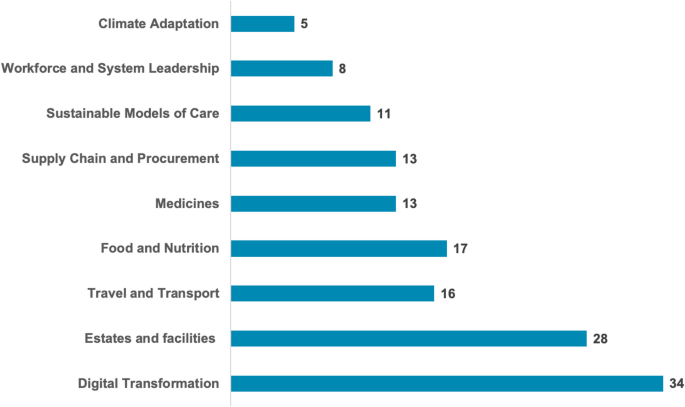
Number of healthcare organizations addressing key areas of environmental sustainability activities
Digital transformation emerges as the most developed area, with 34 organizations actively engaged in its implementation (97%). This reflects a strong focus on expanding the use of telemedicine for remote care and adopting digital systems to reduce reliance on paper records, printing, and postage. These initiatives not only contribute to environmental sustainability but also generate significant cost savings by reducing material usage and administrative expenses. The second most prioritized area is estates and facilities, with 28 organizations reporting active work in this domain (80%). Efforts in this area often focus on improving energy efficiency, reducing energy usage, decarbonizing heating and hot water systems, and adopting waste reduction strategies, including circular economy principles. These initiatives are instrumental in addressing the carbon footprint of healthcare infrastructure while simultaneously reducing operational costs, particularly in energy consumption and waste management. Food and nutrition follow, with 17 organizations involved (49%) in reducing food waste and promoting healthier, locally sourced, and seasonal menus that emphasize plant-based options. This reflects growing recognition of the link between dietary practices and environmental sustainability. Similarly, travel and transport are prioritized by 16 organizations (46%), focusing on increasing active travel and public transport options, as well as investing in low-emission or zero-emission vehicles. These measures also contribute to cost savings by optimizing fleet management and promoting more sustainable modes of transportation. Supply chain and procurement, along with medicines, are addressed by 13 organizations each (37%). In the context of supply chains, efforts aim to reduce the use of clinical and non-clinical single-use plastics, resulting in lower procurement costs and waste management expenses. Initiatives in the area of medicines focus on optimization and waste reduction, responsible disposal, and the consideration of lower-carbon alternatives, all of which can reduce inefficiencies and associated costs. Sustainable models of care are being developed by 11 organizations (31%), emphasizing care delivery closer to home and a preference for lower-carbon interventions when clinically equivalent. These models are not only environmentally beneficial but can also minimize costs related to patient transportation and resource-intensive treatments. Workforce and system leadership, selected by eight organizations (23%), reflects efforts to establish sustainability committees, working groups, and staff training programs on sustainability topics. Although less directly tied to cost savings, these initiatives help embed a culture of sustainability, which can lead to more efficient resource use in the long term. Finally, climate adaptation is the least developed area, with only five organizations (14%) reporting actions such as planning to mitigate the effects of flooding or heatwaves on infrastructure, patients, and staff. While these measures often require significant upfront investment, they have the potential to prevent costly disruptions in the future.
Figure 2 illustrates the distribution of the number of environmental sustainability strategy areas addressed by healthcare organizations, highlighting the extent of multi-dimensional engagement.
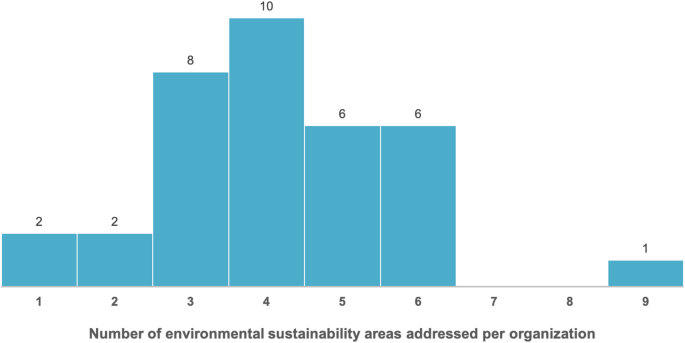
Distribution of the number of environmental sustainability strategy areas addressed by healthcare organizations
The image highlights that the majority of healthcare organizations concentrate on approximately four areas when implementing environmental sustainability practices, as reflected by the mean (4.15) and median [4]. This represents a relatively narrow scope compared to the maximum potential engagement across the nine areas proposed in the questionnaire. Notably, 25% of the organizations demonstrate a more systemic approach to environmental sustainability, addressing more than five areas. However, it is important to note that the breadth of their engagement is not always reflected in their strategic documents, as elaborated in the related section.
With regard to the types of actions undertaken for environmental sustainability strategies by healthcare organizations, the results reveal a certain heterogeneity in the concreteness of the activities. The most commonly undertaken activity is the identification of objectives and priorities for making the organization environmentally sustainable, reported by 22 organizations (62.9%). This suggests that setting strategic goals is perceived as a foundational step in addressing sustainability. The development of monitoring systems, such as quantitative indicators (e.g., CO2 emissions) or qualitative ones (e.g., awareness initiatives), was the second most frequent activity, undertaken by 16 organizations (45.7%). The creation of SMART actions—those that are specific, measurable, achievable, relevant, and time-bound—focused on initial efforts to reduce environmental impacts, and broad engagement with internal and external stakeholders were both reported by 15 organizations (42.9%). On average, each organization has implemented two actions (mean = 2), with a standard deviation of 0.998, indicating some variation in the extent of engagement across organizations.
Figure 3 offers an integrated overview of how healthcare organizations engage with ES, based on two dimensions: the breadth of their approach, measured by the number of ES areas addressed (x-axis), and the depth of their engagement, reflected by the number of actions implemented (y-axis). Each bubble represents one or more organizations, with the size of the bubble indicating how many organizations share that specific position. Bubbles including at least one organization with a dedicated sustainability team are shown in orange, while all others are displayed in blue. The green-shaded area highlights organizations exhibiting broader and more structured ES engagement.
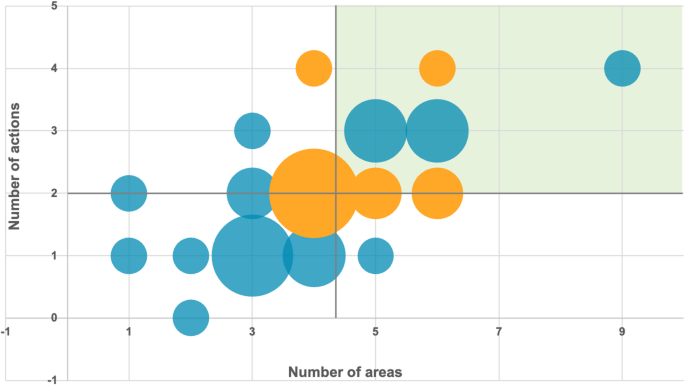
Positioning of healthcare organizations based on the breadth and depth of environmental sustainability implementation. The x-axis represents the number of ES areas addressed (ranging from 0 to 9), while the y-axis indicates the number of concrete actions implemented (ranging from 0 to 4). Bubble size corresponds to the number of organizations. The green-shaded area denotes higher levels of both breadth and concreteness in ES engagement
The analysis reveals a direct association between the number of areas addressed and the number of actions implemented. Organizations engaging across a broader range of areas also tend to undertake a greater number of concrete actions. A cluster of organizations appears in the middle of the graph, representing those that have addressed a moderate number of areas and undertaken a limited set of concrete actions. These organizations suggest a balanced but relatively restrained approach to environmental sustainability, focusing on a manageable scope without fully embedding or operationalizing their strategies. Notably, a smaller group of organizations is positioned in the upper-right quadrant, indicating both a broad engagement across multiple areas and a higher level of concrete action. Regarding the presence of dedicated sustainability teams, the findings suggest that while the establishment of such structures does not automatically guarantee an advanced level of implementation, it appears to represent a positive initial step. Organizations with dedicated teams tend to display intermediate to high levels of activity: notably, 2 organizations with a dedicated team report the maximum number of actions implemented (4 actions), while others demonstrate good coverage across 4 to 4 ES areas.
Barriers and drivers in implementing ES activities
The survey findings highlight several key drivers for environmental sustainability in healthcare organizations, which were gathered through an open-ended question. In contrast, the barriers, derived from those emerging in the literature, were systematically evaluated by the participants in terms of importance. A fundamental driver is the recognition of the close link between environmental health and public well-being. Several respondents stressed that sustainable practices are essential not only for reducing the environmental footprint of healthcare services but also for promoting long-term public health benefits. As one participant noted: “Environmental sustainability is not just about saving energy; it is about reducing the future burden on the healthcare system by promoting healthier environments”. In this perspective, healthcare organizations are increasingly seen as central actors in advancing public health, with a responsibility to lead by example. Economic factors also emerge as a significant driver. Participants emphasized the potential for cost savings through initiatives such as energy efficiency improvements, waste reduction, and resource optimization. One respondent highlighted: “Investments in sustainability, such as solar panels and LED systems, are not only ethically right but also economically strategic, significantly reducing operational cost”. These economic benefits are often coupled with enhanced operational efficiency, as more sustainable practices—such as energy conservation and waste reduction—often streamline processes and reduce wasteful expenditures. This not only improves financial sustainability but also strengthens an organization’s competitive position within the healthcare sector. Furthermore, sustainability is seen as a means of fostering innovation and gaining a competitive advantage. Many respondents pointed out that adopting sustainable practices allows for the development of new healthcare delivery models and technologies, which can enhance service quality and patient care. Hospitals that embrace sustainability are also viewed more favorably by environmentally conscious patients, staff, and investors, helping them to attract talent and build stronger relationships with key stakeholders. In this sense, sustainability is also a driver of reputation and organizational growth. Regulatory compliance is another critical driver for promoting environmental sustainability. Adhering to international and national environmental standards, such as the Kyoto Protocol and the “Do No Significant Harm” (DNSH) principle under the National Recovery and Resilience Plan (NRRP), is crucial for healthcare organizations. A participant remarked: “Meeting environmental regulations is essential not only to avoid sanctions but to build community trust and credibility.” Compliance with these regulations ensures that organizations meet their legal obligations while simultaneously improving their public image and gaining trust from the community. Lastly, there is a strong emphasis on corporate social responsibility (CSR), with top management viewing sustainability as an ethical obligation and a strategic investment for future generations. As one respondent succinctly put it: “Sustainability is not just a project; it is part of our mission to care for people and the planet at the same time.” This commitment not only enhances the organization’s image but also fosters a sense of pride and engagement among employees and stakeholders. By viewing sustainability as a long-term investment, healthcare organizations recognize that their actions today will have lasting impacts on the environment and public health, helping to ensure a healthier, more sustainable future.
Table 4 presents the perceived relevance of each barrier identified by participants in relation to the implementation of environmental sustainability strategies (ESS) within their respective organizations.
The analysis of perceived barriers to the implementation of ES activities reveals a relatively balanced distribution of scores, indicating that healthcare organizations face multiple, interrelated challenges rather than a single dominant obstacle. Although the collection of environmental data received the highest average score (6.92), followed closely by the lack of an organizational monitoring system (6.66), the differences across all barriers are moderate, with average scores ranging from 5.61 to 6.92 on a 10-point scale. This narrow range suggests that respondents perceive these barriers as similarly relevant, reflecting the complexity of integrating ES into healthcare settings where technical, organizational, cultural, and contextual factors interplay. For instance, while data-related issues (collection effort and monitoring systems) emerged as slightly more pressing, other factors—such as competing priorities (6.42), absence of political mandates (6.39), and limited awareness or perceived value among staff (6.16)—also represent substantial hindrances. Furthermore, the standard deviation values, generally above 2.0, highlight a degree of variability in perceptions across organizations, likely influenced by differences in internal capacities, governance structures, and levels of familiarity with sustainability practices.
link





